The Genetic Code Behind Heart Disease
“We are bringing the future of medicine to the patient’s bedside. Targeting health care to the unique genetic make-up of the child will make treatments safer, more effective and precise,” says Dr. Seema Mital, Head of Cardiovascular Research at The Hospital for Sick Children (SickKids) and Scientific Co-lead, Ted Rogers Centre for Heart Research.Mital, who is also a Professor of Paediatrics at the University of Toronto, has launched the first Cardiac Precision Medicine Program in the country focused on deciphering the genetic code of heart disease in children. This knowledge will be used to develop targeted therapies that will help the heart adapt – and prevent patients from developing heart failure in the future.
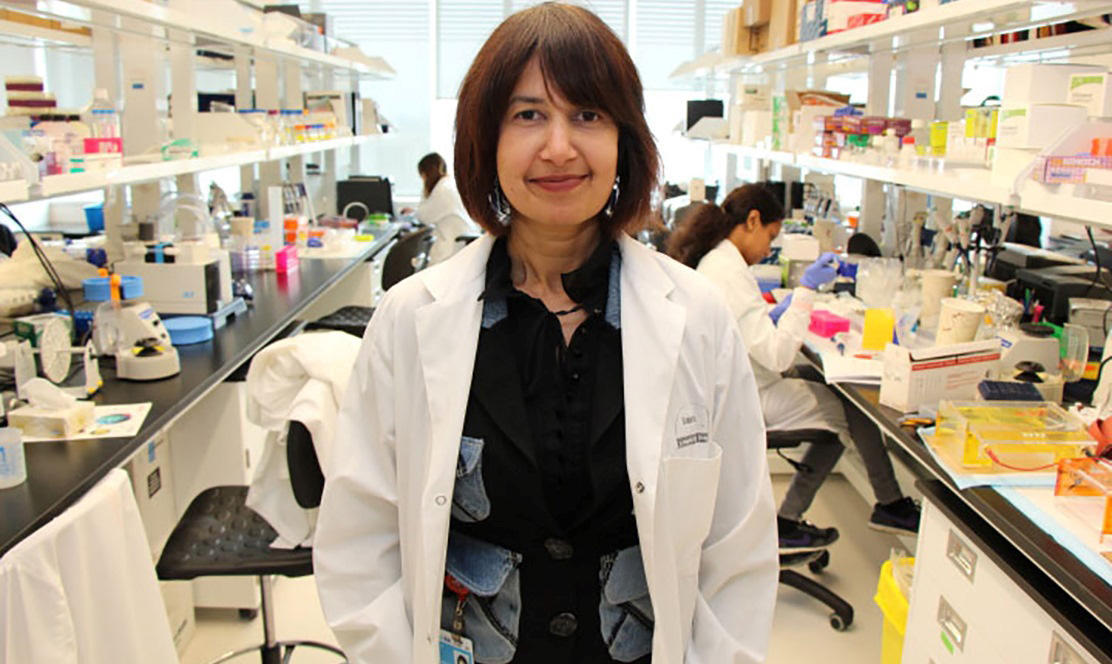
"We need to find ways to either prevent or treat heart failure in children that are more effective than the current ‘one size fits all’ approach."
Since the establishment of the Ted Rogers Centre for Heart Research – a collaborative initiative between SickKids, University Health Network (UHN) and the University of Toronto (U of T) – one year ago, Mital and her team at the Cardiac Precision Medicine Program have been analyzing the genes that predispose patients to two conditions. The first is right ventricle failure in children with Tetralogy of Fallot (the leading cause of 'blue baby' syndrome); the second is cardiomyopathy, a disease that affects the heart’s ability to contract.
While 'blue baby' syndrome can be treated early on with surgical intervention, these children live with leaky valves that eventually cause their heart to fail. SickKids researchers are exploring the genes that predispose infants to right ventricle failure, in the hope of developing new drugs to treat the condition before it becomes irreversible.
Cardiomyopathy (CMP) is a disease of the heart muscle that can cause dangerous forms of irregular heart rate, and sudden cardiac death. There is currently no cure for CMP. Significant developments have been made in genetically diagnosing CMP, although the manner in which gene defects influence patient outcomes is still unknown. In order to find new therapies, Mital is working to generate heart cells from the skin or blood of patients with heart disease. These cells are used to screen drugs before they are tested with patients.
Precision medicine is beginning to change the way we treat patients. Treatment that is directed towards the underlying cause of disease, rather than just the symptoms of disease, will lead to more timely and effective cures – before the condition becomes irreversible.
“The Ted Rogers Centre is facilitating newer, faster and better ways of reaching our goals by catalyzing opportunities and galvanizing researchers to work together to try and find cures for heart failure,” says Mital.