Homegrown Innovation
In healthy lungs, oxygen passes to the blood via millions of miniscule air sacs, more delicate than a soap bubble. In patients with severe complications of COVID-19, these sacs (alveoli) get gummed up with fluid and collapse. Breathing becomes futile. Organs begin to fail. This form of acute respiratory distress syndrome (ARDS) is the worst-case scenario for COVID-19 patients. They are kept alive on a ventilator, which pushes air into the lungs with enough pressure to inflate the alveoli and keep oxygen flowing through the body until—hopefully—the virus subsides.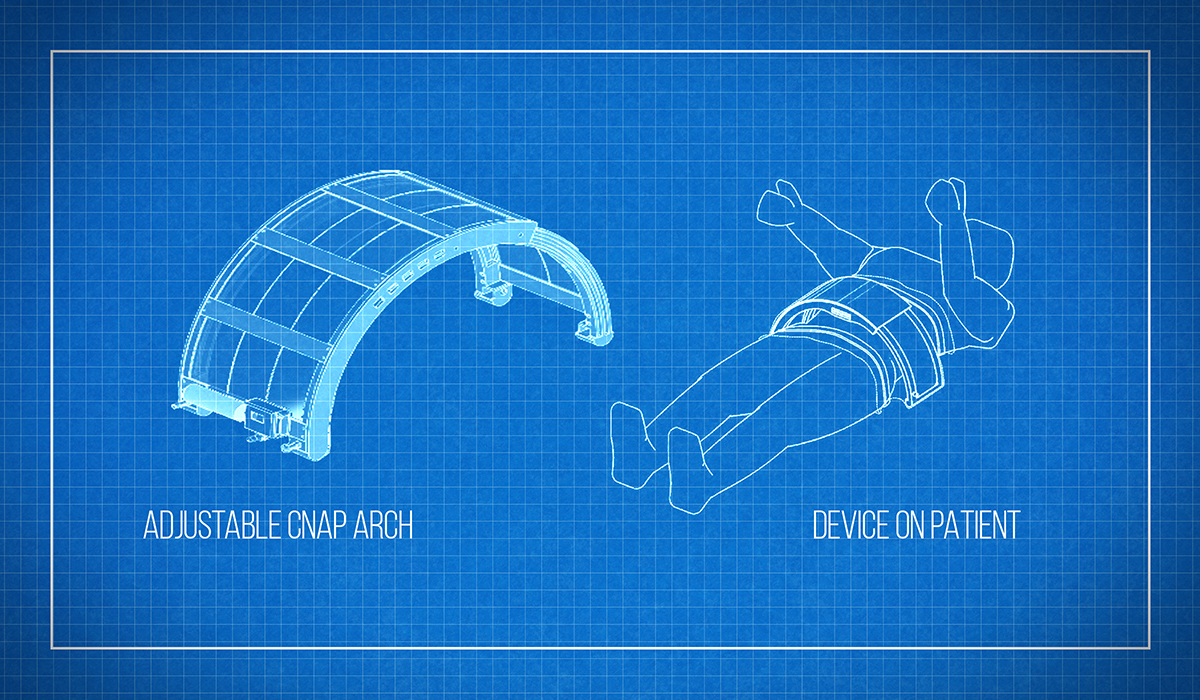
Mechanical ventilation is a lifesaving, though limited technology. Too much pressure can further damage the fragile sacs, while healthy parts of the lung get overstretched and injured, which all works to exacerbate ARDS and can even cause death. For survivors, ventilator damage can be irreversible.
To avoid all this, a team of physicians and engineers at SickKids has designed and built a gentler way to help patients breathe. Whereas standard hospital ventilators use positive pressure, pushing air and oxygen directly into the lungs, the SickKids prototype uses negative pressure, applied outside of the body—akin to iron lung technology used to treat polio. “But instead of enclosing the entire body like the iron lung, ours is a plexiglass arch covering just the abdomen,” says Dr. Martin Post, the SickKids senior scientist who’s leading the project.
As the name implies, the Continuous Negative Abdominal Pressure (CNAP) device moves air in and out of this abdominal chamber, generating negative pressure inside the abdomen. This pulls the diaphragm downward, creating a vacuum inside the chest cavity, which induces the patient to draw air and inflate the lungs. (Similar to how a syringe draws fluid when you pull the plunger.)
CNAP was the brainchild of the late Dr. Brian Kavanagh, a long-time SickKids critical care physician who’d spent much of his career researching ventilator lung damage and better ways to treat ARDS, a common ICU condition with a 40 per cent mortality rate. Over the last decade, he and his team had designed, developed, and tested several CNAP prototypes, all built in-house at our Centre for Image-Guided Innovation and Therapeutic Intervention (CIGITI).
In early preclinical trials, CNAP distributed oxygen more evenly throughout the lungs than standard ventilation, and increased blood oxygen concentrations by up to 20 per cent.
In 2019, just as the team was cleared by Health Canada to trial CNAP in patients at St. Michael’s Hospital, Dr. Kavanagh died following a long illness. Dr. Post planned to continue the study, but when COVID-19 hit, he modified the clinical trial application, proposing to test CNAP on COVID ARDS patients on ventilators.
“The idea is to combine positive and negative pressure in a way that is gentler to the patient, reduces lung damage, and gets them off the ventilator sooner,” says Dr. Post. Within 24 hours, Health Canada approved the trial.
As you read this, a team of engineers and 3D-printing technicians at CIGITI is rushing to build 10 CNAP machines for trials at St. Michael’s and the UHN. At the same time, the team is designing a nimbler prototype for mass manufacturing. The COVID-19 trial, set to begin in a few weeks, will be CNAP’s first true test. If it passes, CNAP may well become the standard, even standalone, treatment for the enduring problem of respiratory failure, well after COVID-19 subsides.
To avoid all this, a team of physicians and engineers at SickKids has designed and built a gentler way to help patients breathe. Whereas standard hospital ventilators use positive pressure, pushing air and oxygen directly into the lungs, the SickKids prototype uses negative pressure, applied outside of the body—akin to iron lung technology used to treat polio. “But instead of enclosing the entire body like the iron lung, ours is a plexiglass arch covering just the abdomen,” says Dr. Martin Post, the SickKids senior scientist who’s leading the project.
"The idea is to combine positive and negative pressure in a way that is gentler to the patient, reduces lung damage, and gets them off the ventilator sooner"
CNAP was the brainchild of the late Dr. Brian Kavanagh, a long-time SickKids critical care physician who’d spent much of his career researching ventilator lung damage and better ways to treat ARDS, a common ICU condition with a 40 per cent mortality rate. Over the last decade, he and his team had designed, developed, and tested several CNAP prototypes, all built in-house at our Centre for Image-Guided Innovation and Therapeutic Intervention (CIGITI).
In early preclinical trials, CNAP distributed oxygen more evenly throughout the lungs than standard ventilation, and increased blood oxygen concentrations by up to 20 per cent.
In 2019, just as the team was cleared by Health Canada to trial CNAP in patients at St. Michael’s Hospital, Dr. Kavanagh died following a long illness. Dr. Post planned to continue the study, but when COVID-19 hit, he modified the clinical trial application, proposing to test CNAP on COVID ARDS patients on ventilators.
“The idea is to combine positive and negative pressure in a way that is gentler to the patient, reduces lung damage, and gets them off the ventilator sooner,” says Dr. Post. Within 24 hours, Health Canada approved the trial.
As you read this, a team of engineers and 3D-printing technicians at CIGITI is rushing to build 10 CNAP machines for trials at St. Michael’s and the UHN. At the same time, the team is designing a nimbler prototype for mass manufacturing. The COVID-19 trial, set to begin in a few weeks, will be CNAP’s first true test. If it passes, CNAP may well become the standard, even standalone, treatment for the enduring problem of respiratory failure, well after COVID-19 subsides.